Team Aims to Transform Care for Diffuse Intrinsic Pontine Glioma
Team Aims to Transform Care for Diffuse Intrinsic Pontine Glioma
Two federal grants are supporting efforts at Children’s Hospital Los Angeles to develop novel therapies for this aggressive childhood brain tumor
LOS ANGELES--(BUSINESS WIRE)--Researchers at Children’s Hospital Los Angeles have received a nearly $1 million K08 grant from the National Institutes of Health (NIH)—as well as funding from the U.S. Department of Defense—to support studies into diffuse intrinsic pontine glioma (DIPG), a childhood brain tumor with a 0% survival rate.
The studies —led by pediatric neurosurgeon Peter Chiarelli, MD, DPhil, and Senior Scientist Meenakshi Upreti, PhD, in the Division of Neurosurgery—are investigating a novel way to improve radiation therapy against DIPG, as well as how to more specifically target the cancer from a molecular standpoint.
DIPG tumors are highly aggressive and grow “by invasion,” interlaced with the normal cells of the critical brainstem. This makes them impossible to surgically remove.
“Since surgery can’t make a dent in this devastating disease, our lab is combining techniques from materials science, chemistry, molecular biology and genetics to find innovative ways to treat these tumors,” Dr. Chiarelli says.
Transforming radiation therapy
The five-year grant from the NIH National Institute of Neurological Disorders and Stroke will support the team’s studies into using nanoparticles to boost—and potentially transform—the effectiveness of radiation therapy.
Peter Chiarelli, MD, DPhil
Radiation therapy is currently the standard of care for DIPG and the only treatment shown to prolong survival for these children. But while it can shrink tumors temporarily, it’s not enough to eliminate them.
To improve these results, Dr. Chiarelli and Dr. Upreti are studying novel nanoparticles—1,000 times smaller than the average human cell—in preclinical models of DIPG. The nanoparticles are designed to find tumors based on a specific marker the cancer cells have on their surface.
Although nanoparticles have mostly been studied in medicine as a way to deliver drugs to specific targets, the researchers are taking a unique approach. They have developed nanoparticles made up of clusters of different metal atoms at their core, surrounded by a biocompatible polymer shell.
The team is testing different forms of these nanoparticles, as well as targeting agents, to see if they can successfully deliver functional materials into DIPG tumor cells. The idea is that the targeted materials will enhance the potency and diminish the risk associated with standard radiation. The goal is to intensify therapeutic effects only within tumor cells—while guarding normal healthy cells from radiation.
“This would be a paradigm shift in therapy if we could use targeted materials to enable this high-impact radiation to select only for tumor cells,” Dr. Chiarelli explains. “That could make radiation therapy more powerful but also safer at the same time.”
Miniaturized models
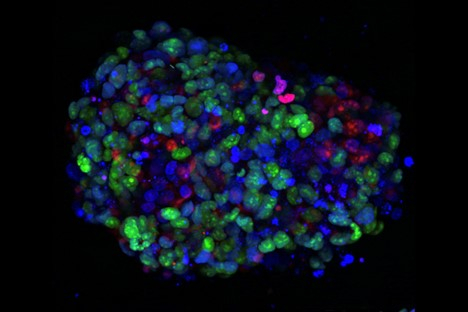
The team is also focused on understanding the critical microenvironment where DIPG tumors reside. The researchers have developed miniaturized models of the tumors—called tumor tissue analogues—that simulate this microenvironment.
Meenakshi Upreti, PhD
“We have made these tumor tissue analogues in many different formulations,” Dr. Chiarelli says. “What we’ve found is that they produce a radically different microenvironment than the one that forms from standard tumor cells in a dish. This is a much more realistic model.”
The investigators will ultimately incorporate a 3D microfluidic culture platform that faithfully captures the characteristics of the DIPG microenvironment. This 3D culture system will allow them to monitor the growth of tumors in real time and see how that microenvironment helps them survive.
Their innovative project has recently received support from the Concept Award from the U.S. Department of Defense Rare Cancers Research Program, as well as from private foundations.
“The idea is to use these tumor tissue analogues in this high-throughput platform, where we could screen hundreds of different drugs and treatment approaches, all at the same time,” he explains. “We particularly want to test newer treatments, such as targeted therapies, immunotherapies and viral vector therapies.”
Aiming for a clinical trial
The ultimate goal for Dr. Chiarelli and Dr. Upreti is to translate their findings into clinical trials for patients in the next five years.
“This is a disease that arises in otherwise healthy children, typically between the ages of 5 and 9,” he says. “It’s devastating to families, and there’s a tremendous need for new therapies and approaches.”
He adds that the lab has benefited from a strong collaboration with senior mentor Rex Moates, PhD, at CHLA. Another key to success? Philanthropic support from families whose children have been treated by Dr. Chiarelli.
“Their generosity has provided vital bridge and seed funding that continues to help propel our studies to the next level and secure federal funding,” Dr. Chiarelli says. “We are extremely grateful for their support and commitment to improving the lives of children with this cancer.”
Contacts
Lorenzo Benet: lbenet@chla.usc.edu