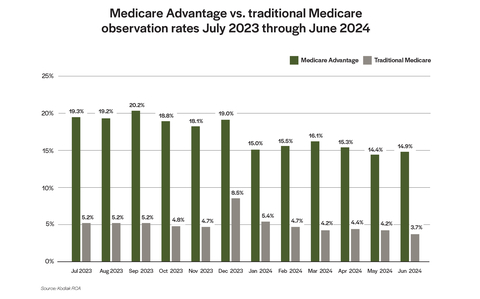
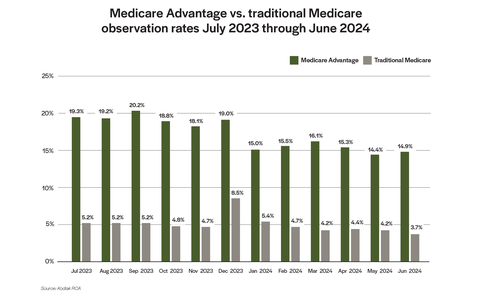
INDIANAPOLIS--(BUSINESS WIRE)--A new analysis of claims data from more than 1,900 hospitals shows that Medicare Advantage plans classified three to four times as many hospital stays as observation visits from July 2023 through the end of June 2024 when compared with traditional Medicare, according to Kodiak Solutions.
Proprietary data from Kodiak Solutions show that MA plans began classifying fewer stays as observation visits starting in January 2024, when a new federal regulation required MA plans to offer their members the same covered services received by beneficiaries in traditional, fee-for-service Medicare. Observation rates for MA plans ranged between 18.1% to 20.2% of claims in the last six months of 2023, then fluctuated within a lower range of 14.4% and 16.1% in the first six months of 2024.
Observation rates in traditional Medicare also trended down over this 12-month period, but within a much lower range of 5.2% to 3.7%, with the exception of a spike to 8.5% in December 2023.
“The gap in observation rates between MA plans and traditional Medicare suggests that MA plans are not fully complying with the federal rule requiring MA plans to offer members the same coverage as traditional Medicare,” said Matt Szaflarski, Director, Revenue Cycle, for Kodiak Solutions. “Our data show the MA observation rates are similar to the rates among patients covered by commercial insurance and, of course, most of the MA plans are also providers of commercial insurance.”
Two-Midnight Rule comes to MA
Whether a patient’s care is classified as an observation stay or an inpatient admission has no effect on the care delivered to the patient. For hospitals, however, the classification is important, as it affects the amount Medicare or an MA plan pays to the hospital, often significantly.
A decade ago, the Centers for Medicare & Medicaid Services (CMS) implemented the Two-Midnight Rule to help hospitals, physicians and Medicare auditors determine whether to classify patient encounters as observation stays or inpatient admissions. Under this rule, when a patient meets certain clinical conditions and the attending or admitting physician believes the patient will stay in the hospital for a period of time that will span at least two midnights, the patient’s care should be classified as an inpatient admission.
Last year, CMS finalized a rule that made clear that MA plans need to cover the same services as traditional Medicare. CMS highlighted the Two-Midnight Rule as an example where MA plans need to provide comparable coverage.
Combatting observation-related denials
Hospitals need to closely monitor payor behaviors across all lines of business regarding observation stays, Szaflarski says.
“Provider organizations should reinforce their denial management practices to ensure that documentation and case reviews are optimized to reduce the opportunity for MA plans to reclassify claims as observation visits,” Szaflarski says.
Revenue cycle leaders also should be on the lookout for the worst examples of these reclassifications to share with their advocacy organizations, Szaflarski adds.
Kodiak Solutions’ data analysis supports the advocacy positions of the American Hospital Association (AHA) and the Federation of American Hospitals (FAH) on how MA plans are implementing the Two-Midnight Rule. In a recent report on hospitals’ rising administrative costs, the AHA cited the growing time and expense of appealing and overturning inappropriate claim denials by MA plans as a leading cause.
To learn more about the data and insights Kodiak Solutions can provide to benchmark your revenue cycle performance, contact Szaflarski at (463) 270-8123.
About Kodiak Solutions
Kodiak Solutions is a leading technology and tech-enabled services company that simplifies complex business problems for healthcare provider organizations. For nearly two decades as a part of Crowe LLP, Kodiak created and developed our proprietary net revenue reporting solution, Revenue Cycle Analytics. Kodiak also provides a broad suite of software and services in support of CFOs looking for solutions in financial reporting, reimbursement, revenue cycle, risk and compliance, and unclaimed property. Kodiak’s 450 employees engage with more than 1,900 hospitals and 250,000 practice-based physicians, across all 50 states, and serve as the unclaimed property outsourcing provider of choice for more than 2,000 companies. To learn more, visit our website.