BOSTON--(BUSINESS WIRE)--Zelis, a leading provider of healthcare technology solutions, announced today the launch of SmartShopper Propel, an omnichannel member engagement and activation solution designed to help health plans (including commercial, Medicare, and Medicaid) support better member health habits and increase member satisfaction. SmartShopper Propel is backed by intelligent consumer-focused engagement strategies and proven incentivization capabilities.
SmartShopper Propel is a natural evolution and addition to Zelis’ best-in-class care redirection solution, SmartShopper, which has provided more than $31 million in cash incentives to participating health plan members in the last six years. The new solution encourages members to take actions aligned to their health plans’ programs for improved health, lower administrative costs, and member engagement. Recent data on the impact of timely preventative care and care for chronic conditions points to the need for a solution like SmartShopper Propel to help health plans streamline the experience for all parties. A shocking 44% of members don’t get the care they need due to difficulties navigating the healthcare landscape.
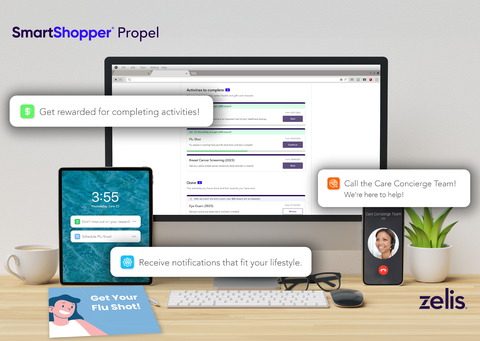
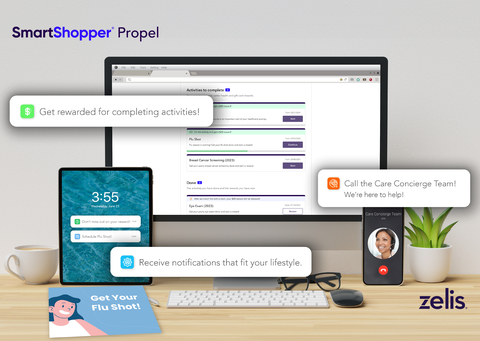
SmartShopper Propel activates members to better navigate the healthcare landscape and learn about open opportunities for care based on their health plan’s goals and programs. Members can receive broad health education and support backed by the top-rated SmartShopper Care Concierge Team. SmartShopper Propel utilizes a multi-channel communication engagement strategy so members can get the information they need when they need it.
“Our clients saw how well incentives worked through SmartShopper and wanted to go a step further and apply it to member activation,” said Heather Cox, President of Insights and Empowerment at Zelis. “With SmartShopper Propel, we are not just presenting members with arbitrary options. We are partnering with health plans to help them reach their member activation goals by creating personalized engagement and incentives tailored to the unique needs of each member.”
Beyond healthcare consumer impact, SmartShopper Propel offers program monitoring of activation and utilization trends among health plan members, ensuring that strategies are tailored to meet goals that will lead to better health outcomes, cost savings for both consumers and health plans, and increased health plan ratings. An example of a use case includes how Propel partners with Medicare plans to activate member programs to help achieve higher quality ratings. This qualifies health plans for bonus payments from CMS and assists Medicaid and Commercial plans to improve their HEDIS scores and member satisfaction.
“SmartShopper Propel was developed in response to our clients’ need for member incentivization, encouraging members to engage with their health plans’ activation and utilization goals,” said Cox. “As the healthcare industry continues to evolve, Zelis remains committed to providing solutions that drive positive change and significantly impact the quality and satisfaction of healthcare experiences for all. SmartShopper Propel represents a giant leap forward in incentivized healthcare member engagement.”
To learn more about SmartShopper Propel, click here.
About Zelis
Zelis is modernizing the healthcare financial experience by providing a connected platform that bridges the gaps and aligns interests across payers, providers, and healthcare consumers. This platform serves more than 700 payers, including the top 5 national health plans, BCBS insurers, regional health plans, TPAs and self-insured employers, and millions of healthcare providers and consumers. Zelis sees across the system to identify, optimize, and solve problems holistically with technology built by healthcare experts – driving real, measurable results for clients. Learn more at Zelis.com and follow us on LinkedIn to get the latest news.