MANHASSET, N.Y.--(BUSINESS WIRE)--Like early pioneers tasked with creating the first geographic maps of the American frontier, scientists at The Feinstein Institutes for Medical Research, supported by a $6.7 million award from the National Institutes of Health (NIH), will create a detailed map of the anatomy of the human vagus nerve – one of the largest and most critical nerves controlling organ functions like heart rate, breathing, digestion, metabolism and immunological responses.
The landmark funding is part of the NIH Common Fund’s Stimulating Peripheral Activity to Relieve Conditions (SPARC) program. The project, called Reconstructing Vagal Anatomy (REVA), will create and ultimately share with the scientific community a map of the anatomical connectivity of vagus nerve fibers from the brainstem, where the vagus nerve starts, all the way down to organs in the neck, chest and abdomen at detail and scope never done before.
The three-year research study is led by the Feinstein Institutes’ Stavros Zanos, MD, PhD; collaborating scientists include Theodoros Zanos, PhD and Larry Miller, MD, from the Feinstein Institutes, Zeinab Nassrallah, PhD from Zucker School of Medicine at Hofstra/Northwell, and Mary Barbe, PhD from Temple University.
“The vagus nerve, with its thousands of sensory and motor fibers, continuously conveys large amounts of information between the brain and peripheral organs and, by doing so, it helps control and coordinate many basic physiological functions,” said Dr. Stavros Zanos, associate professor in the Institute of Bioelectronic Medicine at the Feinstein Institutes. “How sensory and motor fibers are arranged inside the vagus nerve and pathways to different organs are essentially unknown. With the support of the NIH we hope to characterize the nerve’s microscopic structure so that we better understand its function in health and disease, which will ultimately lead to new ways to treat disease with bioelectronic devices through vagus nerve stimulation.”
The vagus nerve, which means “wandering” in Latin, runs from the brainstem to most of the body’s major organs. The nerve is not one solid structure but is instead made up of more than 100,000 sensory and motor fibers, grouped together in several bundles, or fascicles, inside the nerve, eventually forming branches that connect to the organs like the heart, lungs, esophagus, liver and intestines.
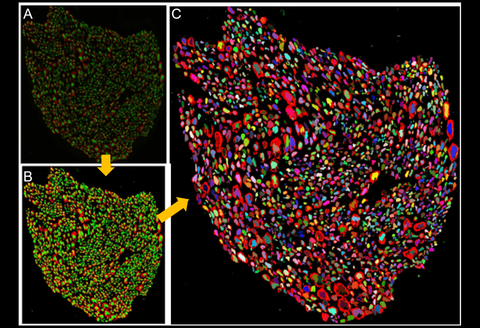
This multi-step research will dissect, image and map the locations and trajectories of the bundles and nerve fibers throughout the length of the vagus nerve and its branches in 60 nerves collected from 30 human cadavers. Next, detailed tomographic imaging will produce detailed, high-definition 3D images. Going microscopic, the team will create a microanatomy atlas of the nerve, staining individual fiber elements and imaging them through a powerful microscope. All of that data will then be correlated and analyzed through artificial intelligence and computer vision algorithms to produce a multi-modal map of the vagus nerve and its fibers in unprecedented detail. This map will then be shared with researchers worldwide.
“The large amounts of data generated by those techniques, along with the need for highly detailed anatomical maps, down to the level of single nerve fibers, makes manual creation of such maps impossible,” said Dr. Theodoros Zanos, associate professor at Feinstein Institutes and the investigator leading the Data Analysis and Visualization (DAVE) core of the program. To properly and efficiently analyze data, we will develop automated methods based on cutting-edge machine learning and computer vision algorithms tailored to this specific application.”
When functioning properly, the vagus nerve contributes to the maintenance of our body’s homeostasis. However, diseases like Crohn’s disease and rheumatoid arthritis, chronic heart diseases, diabetes and even some cancers are associated with inflammation and abnormal vagus nerve function. Through the use of electrical stimulation of the vagus nerve (VNS), researchers at the Feinstein Institutes and elsewhere try to “reset” vagus nerve activity and fight inflammation. The desired and undesired effects of VNS on body functions are determined by how bioelectronic devices stimulate nerve fibers. Knowledge of the detailed arrangement of vagal fibers will contribute to developing more effective and safe VNS devices to fight inflammation, restore homeostatic functions and help treat diseases.
“The vagus nerve is a principal super highway transmitting information in both directions between the brain and body; it can turn on and off our immune system,” said Dr. Tracey, president and CEO of the Feinstein Institutes and Karches Family Distinguished Chair in Medical Research. “This research, led by Dr. Stavros Zanos, generates fundamental new knowledge that will transform our understanding of the human vagus nerve and open new ways to hack the vagus nerve and cure disease with bioelectronic devices.”
The REVA project is supported in part by contract number 75N98022C00019-0-9999-1 from the National Institutes of Health. For more information, go to: https://reporter.nih.gov/project-details/10723189.
About the Feinstein Institutes
The Feinstein Institutes for Medical Research is the home of the research institutes of Northwell Health, the largest health care provider and private employer in New York State. Encompassing 50 research labs, 3,000 clinical research studies and 5,000 researchers and staff, the Feinstein Institutes raises the standard of medical innovation through its five institutes of behavioral science, bioelectronic medicine, cancer, health system science, and molecular medicine. We make breakthroughs in genetics, oncology, brain research, mental health, autoimmunity, and are the global scientific leader in bioelectronic medicine – a new field of science that has the potential to revolutionize medicine. For more information about how we produce knowledge to cure disease, visit http://feinstein.northwell.edu and follow us on LinkedIn.