CAMBRIDGE, Mass. & BEIJING--(BUSINESS WIRE)--BeiGene, Ltd. (NASDAQ: BGNE; HKEX: 06160), a global biotechnology company focused on developing and commercializing innovative medicines worldwide, today announced that BRUKINSA® (zanubrutinib) has received approval from the U.S. Food and Drug Administration (FDA) for the treatment of adult patients with Waldenström’s macroglobulinemia (WM).
“We are delighted by today’s FDA approval for BRUKINSA in its second indication, offering a new treatment option with demonstrated efficacy and safety benefits for patients with Waldenström’s macroglobulinemia. As shown in the ASPEN trial, BRUKINSA can improve treatment outcomes for these patients and potentially make a positive impact on their lives,” commented Jane Huang, M.D., Chief Medical Officer, Hematology at BeiGene.
Dr. Huang continued, “With 11 regulatory approvals in under two years, including two in the U.S., BRUKINSA is demonstrating its growing utility as a treatment option for B-cell malignancies and expanding its footprint to potentially benefit more patients worldwide. We will continue to evaluate BRUKINSA in its broad global clinical program and look forward to additional clinical evidence to establish its position as a potentially best-in-class medicine.”
“The ASPEN trial provided compelling evidence that BRUKINSA is a highly active BTK inhibitor in Waldenström’s macroglobulinemia, and compared to the first-generation BTK inhibitor, showed improved tolerability across a number of clinically important side effects. The approval of BRUKINSA provides an important new option for targeted therapy in Waldenström’s macroglobulinemia,” said Steven Treon, M.D., Ph.D., Director of the Bing Center for Waldenström’s Macroglobulinemia Research at the Dana-Farber Cancer Institute and Professor of Medicine at Harvard Medical School.
“The approval of BRUKINSA in Waldenström’s macroglobulinemia, which is the second therapy approved specifically for the treatment of this rare type of lymphoma, is positive news for patients. Expanded treatment options offer new hope for those living with this disease and can potentially improve patient experience, especially oral therapies that can be given as a single agent,” said Pete DeNardis, Chair of the Board at the International Waldenström’s Macroglobulinemia Foundation (IWMF).
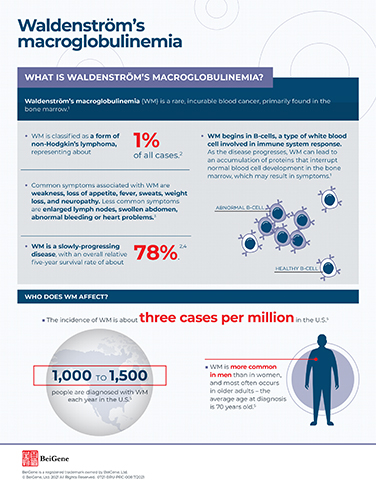
The FDA’s approval of BRUKINSA in WM is primarily based on efficacy results from the multicenter, open-label Phase 3 ASPEN trial (NCT03053440) comparing BRUKINSA to ibrutinib in patients with WM. A total of 201 patients with a MYD88 mutation (MYD88MUT) were enrolled in the randomized Cohort 1.
The primary efficacy endpoint of the ASPEN trial was very good partial response (VGPR) rate in the overall intention-to-treat (ITT) population as assessed by independent review committee (IRC). Based on the modified Sixth International Workshop on Waldenström’s Macroglobulinemia (IWWM-6) response criteria (Treon 2015), the VGPR rate was 28% with BRUKINSA, compared to 19% with ibrutinib; based on the IWWM-6 response criteria (Owen et al 2013), the VGPR rate was 16% with BRUKINSA, compared to 7% with ibrutinib.
In the FDA-approved label, the major efficacy outcome is defined as response rate of partial response (PR) or better as assessed by IRC. Based on either IWWM-6 response criteria, the response rate was 78% with BRUKINSA (95% CI: 68, 85), compared to 78% with ibrutinib (95% CI: 68, 86), and the event-free duration of response (DoR) at 12 months was 94% with BRUKINSA (95% CI: 86, 98), compared to 88% with ibrutinib (95% CI: 77, 94).
The most common (≥20%) adverse reactions based on the pooled safety population of 779 patients were decreased neutrophil count, upper respiratory tract infection, decreased platelet count, rash, hemorrhage, musculoskeletal pain, decreased hemoglobin, bruising, diarrhea, pneumonia, and cough.
The recommended dose of BRUKINSA is either 160 mg twice daily or 320 mg once daily, taken orally with or without food. The dose may be adjusted for adverse reactions and reduced for patients with severe hepatic impairment and certain drug interactions.
About BRUKINSA
BRUKINSA is a small molecule inhibitor of Bruton’s tyrosine kinase (BTK) discovered by BeiGene scientists that is currently being evaluated globally in a broad clinical program as a monotherapy and in combination with other therapies to treat various B-cell malignancies. Because new BTK is continuously synthesized, BRUKINSA was specifically designed to deliver complete and sustained inhibition of the BTK protein by optimizing bioavailability, half-life, and selectivity. With differentiated pharmacokinetics compared to other approved BTK inhibitors, BRUKINSA has been demonstrated to inhibit the proliferation of malignant B cells within a number of disease relevant tissues.
BRUKINSA is approved in the following indications and regions:
- For the treatment of mantle cell lymphoma (MCL) in adult patients who have received at least one prior therapy (United States, November 2019)*;
- For the treatment of MCL in adult patients who have received at least one prior therapy (China, June 2020)**;
- For the treatment of chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) in adult patients who have received at least one prior therapy (China, June 2020)**;
- For the treatment of relapsed or refractory MCL (United Arab Emirates, February 2021);
- For the treatment of Waldenström’s macroglobulinemia (WM) in adult patients (Canada, March 2021);
- Registered and reimbursed for the treatment of MCL in patients who have received at least one prior therapy (Israel, April 2021);
- For the treatment of adult patients with WM who have received at least one prior therapy (China, June 2021)**;
- For the treatment of MCL in adult patients who have received at least one prior therapy (Canada, July 2021);
- For the treatment of adult patients with MCL who have received at least one previous therapy (Brazil, August 2021); and
- For the treatment of adult patients with WM (United States, August 2021).
To-date, more than 30 marketing authorization applications in multiple indications have been submitted in the United States, China, the European Union, and more than 20 other countries or regions.
* This indication was approved under accelerated approval based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
** This indication was approved under conditional approval. Complete approval for this indication may be contingent upon results from ongoing randomized, controlled confirmatory clinical trials.
IMPORTANT U.S. SAFETY INFORMATION FOR BRUKINSA (ZANUBRUTINIB)
Warnings and Precautions
Hemorrhage
Fatal and serious hemorrhagic events have occurred in patients with hematological malignancies treated with BRUKINSA monotherapy. Grade 3 or higher hemorrhage including intracranial and gastrointestinal hemorrhage, hematuria and hemothorax have been reported in 3.0% of patients treated with BRUKINSA monotherapy. Hemorrhage events of any grade occurred in 35% of patients treated with BRUKINSA monotherapy.
Bleeding events have occurred in patients with and without concomitant antiplatelet or anticoagulation therapy. Co-administration of BRUKINSA with antiplatelet or anticoagulant medications may further increase the risk of hemorrhage.
Monitor for signs and symptoms of bleeding. Discontinue BRUKINSA if intracranial hemorrhage of any grade occurs. Consider the benefit-risk of withholding BRUKINSA for 3-7 days pre- and post-surgery depending upon the type of surgery and the risk of bleeding.
Infections
Fatal and serious infections (including bacterial, viral, or fungal) and opportunistic infections have occurred in patients with hematological malignancies treated with BRUKINSA monotherapy. Grade 3 or higher infections occurred in 28% of patients treated with BRUKINSA monotherapy. The most common Grade 3 or higher infection was pneumonia. Infections due to hepatitis B virus (HBV) reactivation have occurred.
Consider prophylaxis for herpes simplex virus, pneumocystis jiroveci pneumonia and other infections according to standard of care in patients who are at increased risk for infections. Monitor and evaluate patients for fever or other signs and symptoms of infection and treat appropriately.
Cytopenias
Grade 3 or 4 cytopenias, including neutropenia (28%), thrombocytopenia (11%) and anemia (7%) based on laboratory measurements, were reported in patients treated with BRUKINSA monotherapy. Grade 4 neutropenia occurred in 13% of patients, and Grade 4 thrombocytopenia occurred in 4% of patients.
Monitor complete blood counts regularly during treatment and interrupt treatment, reduce the dose, or discontinue treatment as warranted. Treat using growth factor or transfusions, as needed.
Second Primary Malignancies
Second primary malignancies, including non-skin carcinoma, have occurred in 13% of patients treated with BRUKINSA monotherapy. The most frequent second primary malignancy was non-melanoma skin cancer, reported in 7% of patients. Other second primary malignancies included malignant solid tumors (4%), melanoma (1.4%), and hematologic malignancies (1.2%). Advise patients to use sun protection and monitor patients for the development of second primary malignancies.
Cardiac Arrhythmias
Atrial fibrillation and atrial flutter have occurred in 2.8% of patients treated with BRUKINSA monotherapy. Patients with cardiac risk factors, hypertension, and acute infections may be at increased risk. Grade 3 or higher events were reported in 0.8% of patients treated with BRUKINSA monotherapy. Monitor signs and symptoms for atrial fibrillation and atrial flutter and manage as appropriate.
Embryo-Fetal Toxicity
Based on findings in animals, BRUKINSA can cause fetal harm when administered to a pregnant woman. Administration of zanubrutinib to pregnant rats during the period of organogenesis caused embryo-fetal toxicity including malformations at exposures that were 5 times higher than those reported in patients at the recommended dose of 160 mg twice daily. Advise women to avoid becoming pregnant while taking BRUKINSA and for 1 week after the last dose. Advise men to avoid fathering a child during treatment and for 1 week after the last dose.
If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
Adverse reactions
The most common adverse reactions including laboratory abnormalities in ≥20% of patients who received BRUKINSA (N = 779) were decreased neutrophil count (56%), upper respiratory tract infection (49%), decreased platelet count (44%), rash (35%), hemorrhage (35%), musculoskeletal pain (30%), decreased hemoglobin (28%), bruising (25%), diarrhea (23%), pneumonia (22%), and cough (21%).
Drug Interactions
CYP3A Inhibitors: When BRUKINSA is co-administered with a strong CYP3A inhibitor, reduce BRUKINSA dose to 80 mg once daily. For coadministration with a moderate CYP3A inhibitor, reduce BRUKINSA dose to 80 mg twice daily.
CYP3A Inducers: Avoid coadministration with moderate or strong CYP3A inducers.
Specific Populations
Hepatic Impairment: The recommended dose of BRUKINSA for patients with severe hepatic impairment is 80 mg orally twice daily.
Please see full U.S. Prescribing Information at https://www.beigene.com/PDF/BRUKINSAUSPI.pdf and Patient Information at https://www.beigene.com/PDF/BRUKINSAUSPPI.pdf.
BeiGene Oncology
BeiGene is committed to advancing best and first-in-class clinical candidates internally or with like-minded partners to develop impactful and affordable medicines for patients across the globe. We have a growing R&D team of approximately 2,300 colleagues dedicated to advancing more than 90 clinical trials involving more than 13,000 patients and healthy volunteers. Our expansive portfolio is directed by a predominantly internalized clinical development team supporting trials in more than 40 countries. Hematology-oncology and solid tumor targeted therapies and immuno-oncology are key focus areas for the Company, with both mono- and combination therapies prioritized in our research and development. We currently market three medicines discovered and developed in our labs: BTK inhibitor BRUKINSA in the United States, China, Canada, and additional international markets; and non-FC-gamma receptor binding anti-PD-1 antibody tislelizumab and PARP inhibitor pamiparib in China.
BeiGene also partners with innovative companies who share our goal of developing therapies to address global health needs. We commercialize a range of oncology medicines in China licensed from Amgen and Bristol Myers Squibb. We also plan to address greater areas of unmet need globally through our collaborations including with Amgen, Bio-Thera, EUSA Pharma, Mirati Therapeutics, Seagen, and Zymeworks. BeiGene has also entered into a collaboration with Novartis granting Novartis rights to develop, manufacture, and commercialize tislelizumab in North America, Europe, and Japan.
About BeiGene
BeiGene is a global, science-driven biotechnology company focused on developing innovative and affordable medicines to improve treatment outcomes and access for patients worldwide. With a broad portfolio of more than 40 clinical candidates, we are expediting development of our diverse pipeline of novel therapeutics through our own capabilities and collaborations. We are committed to radically improving access to medicines for two billion more people by 2030. BeiGene has a growing global team of over 7,000 colleagues across five continents. To learn more about BeiGene, please visit www.beigene.com and follow us on Twitter at @BeiGeneGlobal.
Forward-Looking Statements
This press release contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 and other federal securities laws, including statements regarding BeiGene's plan for the advancement, and anticipated clinical development, regulatory milestones and commercialization of BRUKINSA, the potential for BRUKINSA to provide improved clinical benefits to patients, and BeiGene’s plans, commitments, aspirations, and goals under the headings “BeiGene Oncology” and “About BeiGene”. Actual results may differ materially from those indicated in the forward-looking statements as a result of various important factors, including BeiGene's ability to demonstrate the efficacy and safety of its drug candidates; the clinical results for its drug candidates, which may not support further development or marketing approval; actions of regulatory agencies, which may affect the initiation, timing and progress of clinical trials and marketing approval; BeiGene's ability to achieve commercial success for its marketed medicines and drug candidates, if approved; BeiGene's ability to obtain and maintain protection of intellectual property for its medicines and technology; BeiGene's reliance on third parties to conduct drug development, manufacturing and other services; BeiGene’s limited experience in obtaining regulatory approvals and commercializing pharmaceutical products and its ability to obtain additional funding for operations and to complete the development and commercialization of its drug candidates and achieve and maintain profitability; the impact of the COVID-19 pandemic on the BeiGene’s clinical development, regulatory, commercial, and other operations, as well as those risks more fully discussed in the section entitled “Risk Factors” in BeiGene’s most recent quarterly report on Form 10-Q as well as discussions of potential risks, uncertainties, and other important factors in BeiGene's subsequent filings with the U.S. Securities and Exchange Commission. All information in this press release is as of the date of this press release, and BeiGene undertakes no duty to update such information unless required by law.