WHIPPANY, N.J.--(BUSINESS WIRE)--Bayer announced today that detailed results from the FIDELIO-DKD Phase III study demonstrated that the investigational drug finerenone slowed the progression of chronic kidney disease (CKD) in patients with CKD and type 2 diabetes (T2D) compared to placebo. In the study, finerenone significantly reduced the risk of the composite primary endpoint of time to kidney failure, a sustained decrease of estimated glomerular filtration rate (eGFR) greater than or equal to 40 percent from baseline over a period of at least four weeks, or renal death by 18 percent (relative risk reduction, HR 0.82 [95 percent CI, 0.73-0.93; p=0.0014]) over a median duration of follow-up of 2.6 years when added to maximum tolerated dose of guideline-directed therapy.5 At 36 months, the number needed to treat to prevent a primary composite endpoint event was 29 [95 percent CI 16-166]. FIDELIO-DKD is the first large contemporary positive outcomes study in patients with CKD and T2D with a primary composite endpoint exclusively consisting of kidney-specific outcomes.1,2 The findings from the FIDELIO-DKD study, which is part of the largest Phase III clinical trial program to date in CKD and T2D1,2, were presented today at the virtual American Society of Nephrology’s (ASN) Kidney Week 2020, October 22 – 25, and simultaneously published in the New England Journal of Medicine.
“Despite available treatments focusing on hemodynamic and metabolic pathways, there is residual risk of kidney disease progression in patients with chronic kidney disease and type 2 diabetes.3,6 The findings from FIDELIO-DKD provide important evidence suggesting a potential new strategy for treating these patients,” said Professor George L. Bakris, M.D., Department of Medicine, American Heart Association Comprehensive Hypertension Center, University of Chicago Medicine, U.S. and principal investigator of FIDELIO-DKD. “Overactivation of the mineralocorticoid receptor contributes to inflammation and fibrosis in the kidneys and heart, which represents an unmet medical need. The results with finerenone are highly relevant for these patients who currently have limited options.”
Finerenone also significantly reduced the risk of the key secondary endpoint, a composite of time to cardiovascular death, non-fatal myocardial infarction, non-fatal stroke or hospitalization for heart failure compared to placebo by 14 percent (relative risk reduction, HR 0.86 [95 percent CI, 0.75-0.99; p=0.0339]) over a median duration of follow-up of 2.6 years. Patients in both groups received standard of care, including blood glucose lowering therapies and maximum tolerated dose of RAS-blocking therapy such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs).
“These vulnerable patients need to be protected by delaying the need for dialysis or a kidney transplant and to reduce their risk of cardiovascular events,” said Dr. Joerg Moeller, member of the Executive Committee of Bayer AG's Pharmaceutical Division and Head of Research and Development. “There is a high unmet medical need in cardiovascular and kidney diseases, which we aim to address with our research and development efforts. The FIDELIO-DKD results demonstrate that finerenone may become a new potential therapeutic option for patients with chronic kidney disease and type 2 diabetes.”
Overall treatment-emergent adverse events and serious adverse events were similar between groups. The majority of adverse events were mild or moderate. The frequency of serious adverse events was lower in patients treated with finerenone (31.9 percent) compared to placebo (34.3 percent). Overall hyperkalemia-related adverse events occurred more often in patients receiving finerenone compared with placebo (18.3 percent and 9 percent, respectively). Hyperkalemia-related serious adverse events were 1.6 percent and 0.4 percent, respectively and there was no hyperkalemia-related death in either treatment group. Treatment was discontinued due to hyperkalemia in 2.3 percent of patients treated with finerenone compared to 0.9 percent in the placebo group.
Bayer plans to submit a New Drug Application (NDA) for finerenone to the U.S. Food and Drug Administration (FDA) by end of this year.
About Finerenone
Finerenone (BAY 94-8862) is an investigational, non-steroidal, selective mineralocorticoid receptor antagonist (MRA) that has been shown to reduce many of the harmful effects of mineralocorticoid receptor (MR) overactivation.7 Mineralocorticoid receptor overactivation is a driver of kidney and cardiovascular damage through inflammatory and fibrotic processes.6,8
The Phase III program with finerenone in CKD and T2D randomized 13,000 patients across a broad range of disease severity including those with early kidney damage and more advanced stages of kidney disease. It is the largest Phase III clinical trial program to date in CKD and T2D and comprises two studies, evaluating the effect of finerenone versus placebo on top of standard of care on both renal and cardiovascular outcomes.1,2
FIDELIO-DKD (FInerenone in reducing kiDnEy faiLure and dIsease prOgression in Diabetic Kidney Disease) is a randomized, double-blind, placebo-controlled, parallel-group, multicenter, event-driven Phase III study that investigated the efficacy and safety of finerenone in comparison to placebo in addition to standard of care on the reduction of kidney failure and kidney disease progression in approximately 5,700 patients with CKD and T2D from more than 1,000 sites across 48 countries worldwide. Finerenone 10 mg or 20 mg orally once daily when added to standard of care, including blood glucose lowering therapies and maximum tolerated dose of RAS-blocking therapy such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), significantly reduced the combined risk of time to kidney failure, a sustained decrease of estimated glomerular filtration rate (eGFR) ≥40 percent from baseline over a period of at least four weeks, or renal death by 18 percent (relative risk reduction; HR 0.82 [95% CI, 0.73-0.93; p=0.0014]) over a median duration of follow-up of 2.6 years.
FIGARO-DKD (FInerenone in reducinG cArdiovascular moRtality and mOrbidity in Diabetic Kidney Disease) is still ongoing and is investigating the efficacy and safety of finerenone versus placebo in addition to standard of care on the reduction of cardiovascular morbidity and mortality in approximately 7,400 patients with CKD and T2D across 47 countries including sites in Europe, Japan, China and the U.S.
Bayer also recently announced the initiation of the FINEARTS-HF study, a multicenter, randomized, double-blind, placebo-controlled Phase III study which will investigate finerenone compared to placebo in more than 5,500 symptomatic heart failure patients (New York Heart Association class II-IV) with a left ventricular ejection fraction of ≥40 percent. The primary objective of the study is to demonstrate superiority of finerenone over placebo in reducing the rate of the composite endpoint of cardiovascular death and total (first and recurrent) heart failure (HF) events (defined as hospitalizations for HF or urgent HF visits).
About Chronic Kidney Disease in Type 2 Diabetes
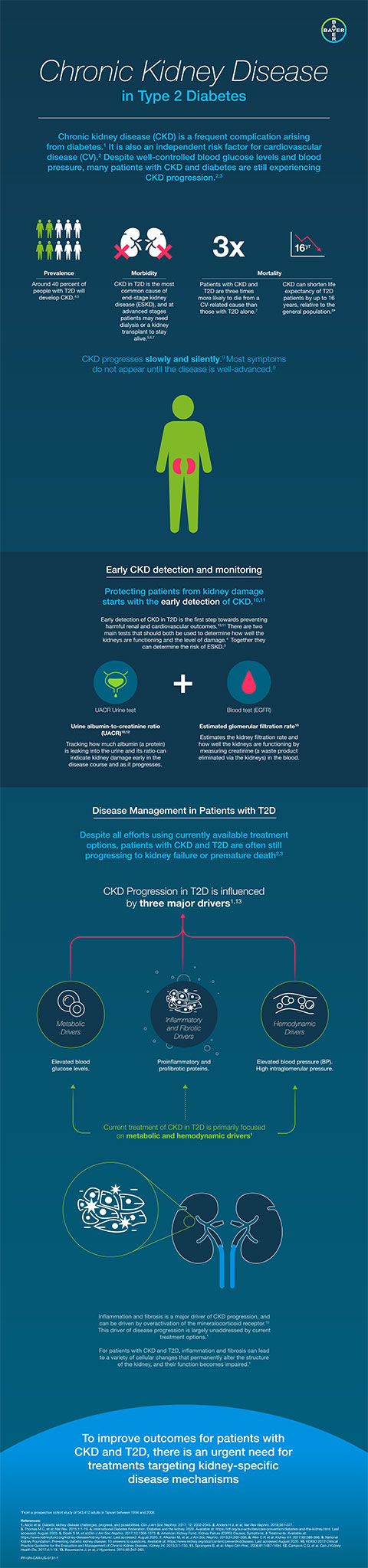
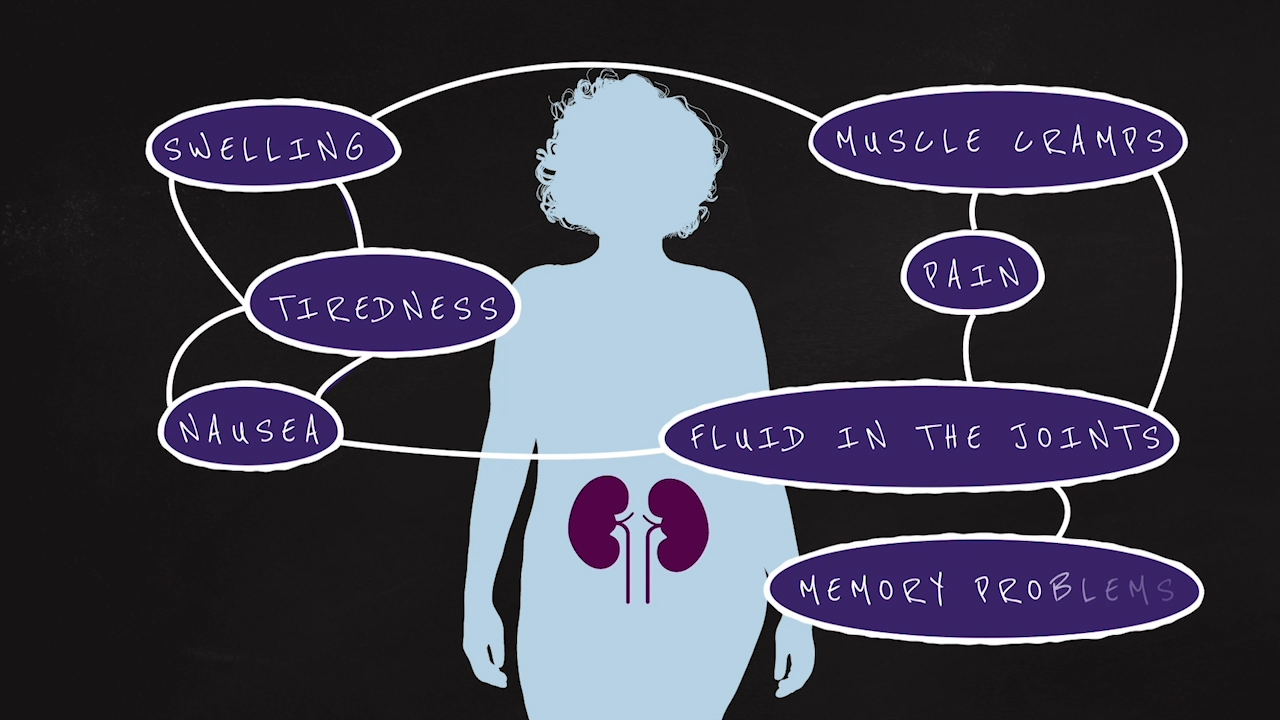
Chronic kidney disease is a life-threatening condition that is underrecognized. CKD is one of the most frequent complications arising from diabetes and is also an independent risk factor of cardiovascular disease.3 Approximately 40 percent of all patients with T2D develop CKD.9 Despite guideline-directed therapies, patients with CKD and T2D remain at high risk of CKD progression and cardiovascular events.3,4 In 2013, diabetes led to more than 51,000 new cases of kidney failure in the U.S.10 Chronic kidney disease in T2D is the main cause of end stage kidney disease11 and kidney failure and at advanced stages, patients may need dialysis or a kidney transplant to stay alive.12 Mineralocorticoid receptor over-activation is known to trigger detrimental processes (e.g., inflammation and fibrosis) in the kidneys and heart in patients with CKD and T2D.6
About Bayer’s Commitment in Cardiovascular and Kidney Diseases
Bayer is an innovation leader in the area of cardiovascular diseases, with a long-standing commitment to delivering science for a better life by advancing a portfolio of innovative treatments. The heart and the kidneys are closely linked in health and disease, and Bayer is working in a wide range of therapeutic areas on new treatment approaches for cardiovascular and kidney diseases with high unmet medical needs. The cardiology franchise at Bayer already includes a number of products and several other compounds in various stages of preclinical and clinical development. Together, these products reflect the company’s approach to research, which prioritizes targets and pathways with the potential to impact the way that cardiovascular diseases are treated.
About Bayer
Bayer is a global enterprise with core competencies in the life science fields of health care and nutrition. Its products and services are designed to benefit people by supporting efforts to overcome the major challenges presented by a growing and aging global population. At the same time, the Group aims to increase its earning power and create value through innovation and growth. Bayer is committed to the principles of sustainable development, and the Bayer brand stands for trust, reliability and quality throughout the world. In fiscal 2019, the Group employed around 104,000 people and had sales of 43.5 billion euros. Capital expenditures amounted to 2.9 billion euros, R&D expenses to 5.3 billion euros. For more information, go to www.bayer.us.
Find more information at www.pharma.bayer.com
Our online press service is just a click away: www.bayer.us/en/newsroom
Follow us on Facebook: http://www.facebook.com/pharma.bayer
Follow us on Twitter: https://twitter.com/BayerUS
Forward-Looking Statements
This release may contain forward-looking statements based on current assumptions and forecasts made by Bayer management. Various known and unknown risks, uncertainties and other factors could lead to material differences between the actual future results, financial situation, development or performance of the company and the estimates given here. These factors include those discussed in Bayer’s public reports which are available on the Bayer website at www.bayer.com. The company assumes no liability whatsoever to update these forward-looking statements or to conform them to future events or developments.
_______________________________________________________________________
1 Data on file.
2 ClinicalTrials.gov. Efficacy and Safety of Finerenone in Subjects with Type 2 Diabetes Mellitus and Diabetic Kidney Disease (FIDELIO-DKD). Accessed October 6, 2020. https://clinicaltrials.gov/ct2/show/NCT02540993.
3 Alicic RZ, et al. Diabetic kidney disease challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12:2032-2045.
4 Pálsson, R, et al. Cardiovascular Complications of Diabetic Kidney Disease. Adv Chronic Kidney Dis. 2014;21(3): 273–280.
5 National Kidney Foundation. KDOQI Clinical Practice Guideline For Diabetes and CKD: 2012 Update. Accessed October 6, 2020. https://www.ajkd.org/article/S0272-6386(12)00957-2/pdf
6 Bauersachs J, et al. Mineralocorticoid receptor activation and mineralocorticoid receptor antagonist treatment in cardiac and renal diseases. Hypertension. 2015 Feb;65(2):257-63.
7 Kolkhof et al. Steroidal and novel non-steroidal mineralocorticoid receptor antagonists in heart failure and cardiorenal diseases: comparison at bench and bedside. Handb Exp Pharmacol. 2017;243:271-305.
8 Buonafine, M et al. Mineralocorticoid Receptor and Cardiovascular Disease. Am J Hypertens. 2018;31(11):1165-1174.
9 International Diabetes Foundation. IDF diabetes atlas 8th edition 2017. Accessed October 5, 2020. https://www.diabetesatlas.org/en.
10 National Kidney Foundation. Diabetes and Chronic Kidney Disease. Accessed October 6, 2020. https://www.kidney.org/news/newsroom/factsheets/Diabetes-And-CKD.
11 Doshi SM et al. Diagnosis and management of type 2 diabetic kidney disease. Clin J Am Soc Nephrol. 2017 Aug 7;12(8):1366-1373.
12 KidneyFund.org. Kidney Failure. Accessed October 6, 2020. https://www.kidneyfund.org/kidney-disease/kidney-failure.