MINNETONKA, Minn.--(BUSINESS WIRE)--UnitedHealthcare’s value-based care program for knee, hip and spine procedures has demonstrated fewer hospital readmissions and complications following surgery, while generating total savings of nearly $18 million for participating employers.
The Spine and Joint Solution helped reduce hospital readmissions by 22 percent and led to 17 percent fewer complications for joint replacement surgeries, as compared to nonparticipating facilities. For spine surgeries, hospital readmissions were reduced by 10 percent, and there were 3.4 percent fewer complications, as compared to nonparticipating facilities.
Since the program’s introduction, participating employers have realized an average savings of $18,000 per operation when compared with median costs in the same metropolitan area. Eligible employees saved more than $3,000 in out-of-pocket costs per procedure when accessing a participating facility rather than another in-network medical facility, with incentives such as cash, gift cards, additional vacation days for recovery, and health savings account (HSA) contributions.
The program’s bundled payment method reimburses health care providers and facilities for a defined episode of care, such as knee or hip replacement, under a single fee or payment. This is a shift away from the traditional fee-for-service structure in which a care provider is paid for each treatment, appointment or test, generating multiple claims within a single, broader episode of care.
The Spine and Joint Solution has expanded nationwide to 46 participating health care facilities, with more than 115 employers enrolled and 3 million employees. The program, available to companies of any size with self-funded health plans, provides employees with access to surgeons and facilities that qualify as UnitedHealthcare Centers of Excellence and accept bundled case rates for knee and hip replacement, spinal fusion and spinal disc repair. All participating health care facilities have been independently evaluated for providing quality patient care and better outcomes.
“This program is one example of the ways we are reshaping how health care is delivered, helping enhance care coordination, improve outcomes and deliver greater value,” said Sam Ho, M.D., chief medical officer of UnitedHealthcare. “The initial results and nationwide expansion demonstrate the value of this program to health care providers, employers and their employees, helping to improve health outcomes and make care more affordable for more people.”
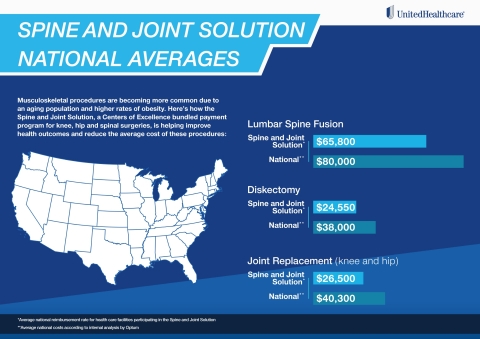
Musculoskeletal procedures are becoming more common due to an aging population and higher obesity rates. Moreover, these procedures are expensive, and costs and outcomes vary widely among care providers.
“Working with UnitedHealthcare on this program has furthered our efforts to treat the whole person, providing patients with access to comprehensive, coordinated care,” said Mark Carley, vice president of managed care and payor relations, Centura Health, which has participated in the Spine and Joint Solution since 2016. “Employers are seeking new ways to enhance employee health and reduce costs. By effectively coordinating patient care among the primary care provider, the surgeon, hospital and health plan, we can improve postoperative care, reduce readmissions, and enhance outcomes and the patient experience, leading to healthier communities.”
The Spine and Joint Solution was developed in collaboration with Optum, a UnitedHealth Group (NYSE: UNH) company.
UnitedHealthcare Value-Based Care Portfolio Continues to Grow
Value-based care models have made tremendous gains in adoption across America’s health care system over the last few years. UnitedHealthcare’s care provider reimbursements that are tied to a variety of value-based care arrangements have nearly tripled in the last three years to $64 billion annually, and are expected to reach $75 billion by the end of 2020.
To date, more than 15 million people, or nearly one in every three people enrolled in UnitedHealthcare benefit plans, currently access care from providers in value-based care relationships.
UnitedHealth Group (NYSE: UNH) recently announced advancements in the company’s collaboration with individual doctors, health systems and governments as the use of bundled payment models expands in traditional fee-for-service Medicare. UnitedHealth Group aims to offer data and analytics, technology and care coordination to support the bundled payment models of health care providers, including those participating in the Centers for Medicare & Medicaid Services (CMS) Bundled Payments for Care Improvement Advanced (BPCI Advanced) program when BPCI Advanced launches later this year.
For more information about Value-Based Care, visit www.uhc.com/valuebasedcare.
About UnitedHealthcare
UnitedHealthcare
is dedicated to helping people live healthier lives and making the
health system work better for everyone by simplifying the health care
experience, meeting consumer health and wellness needs, and sustaining
trusted relationships with care providers. In the United States,
UnitedHealthcare offers the full spectrum of health benefit programs for
individuals, employers, and Medicare and Medicaid beneficiaries, and
contracts directly with more than 1.2 million physicians and care
professionals, and 6,500 hospitals and other care facilities nationwide.
The company also provides health benefits and delivers care to people
through owned and operated health care facilities in South America.
UnitedHealthcare is one of the businesses of UnitedHealth Group (NYSE:
UNH), a diversified health care company. For more information, visit
UnitedHealthcare at www.uhc.com or
follow @UHC on Twitter.
Click here to subscribe to Mobile Alerts for UnitedHealth Group.