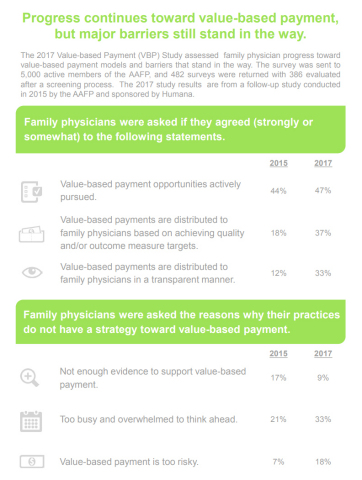
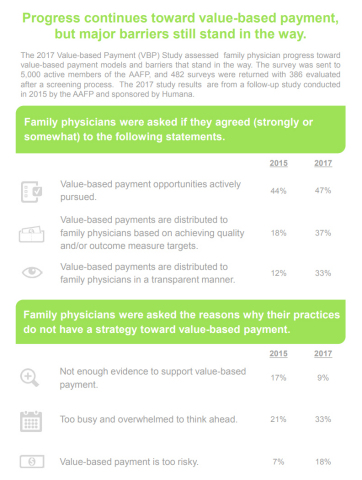
WASHINGTON--(BUSINESS WIRE)--Fifty-four percent of family physicians indicate their practices participate in value-based payment models and half believe value-based payment models will encourage greater collaboration between primary care physicians and specialists. Those are among the key findings from a recent study on physician acceptance of value-based payment. These results are being shared by the American Academy of Family Physicians (AAFP) and Humana Inc. (NYSE: HUM) in a congressional briefing today.
The results are from a follow-up study conducted by the AAFP and sponsored by Humana. The study found that more and more family physicians are embracing value-based payment models, which is reflected in IT, care coordination and other investments. According to the study, family physicians are:
- Acknowledging a connection between quality and payment. Thirty-seven percent of value-based payments distributed within a family physician’s practice are based on achieving quality and/or outcome measures, an increase from 18 percent as reported in 2015.
-
Investing in care coordination as part of their approach to
value-based payment models. Thirty-two percent of family
physicians report that they provide ongoing care
management/coordination services to all high-risk patients, an
increase of 23 percent from 2015.
- Forty-three percent cite hiring/hired care management and care coordinators, compared to 33 percent in 2015.
- Earmarking more practice resources for value-based payment. Fifty-four percent of family physicians are in a practice that is updating or adding health IT infrastructure for data management and analysis to participate in value-based payment.
“Family physicians are doing the work to prepare for value-based care models,” said AAFP President Michael Munger, M.D. “Our members are making changes at the practice level and making investments to prepare for the transition to value-based models that will support better care. However, major barriers still exist that are stifling progress. Among the most commonly noted are issues related to administrative burden like a lack of staff time, lack of standardization for reporting requirements and lack of data transparency. That’s why the AAFP is committed to working on administrative simplification for our members so they can focus more on caring for patients and less on dealing with paperwork. We appreciate Humana’s efforts to partner with us and support family physicians in this effort.”
The same barriers to navigating and implementing value-based payment models that the AAFP and Humana identified two years ago are still prevalent:
- Lack of staff time (90 percent).
- Lack of transparency between payors and providers (78 percent).
- Lack of standardization of performance measures (78 percent).
- No uniform insurance company reports on performance (75 percent).
Additionally, only 8 percent of family physicians agree with the statement “quality expectations are easy to meet in VBP models,” down from 13 percent in 2015.
“The AAFP continues to be an invaluable partner in helping us listen to and better understand primary care physicians and the challenges they face,” said Roy A. Beveridge, M.D., Humana’s Chief Medical Officer. “While the study shows that more family physicians have adopted value-based payments, there’s not much change in the way they see this model of care influencing what they care most about – their patients’ health, or their staffs’ morale and their practices’ performance.” He added that Humana is using these findings to create even greater urgency for its simplification efforts, including standardizing quality measures and reducing the number of them as well as increasing collaboration and transparency in sharing data and actionable insights.
The 2017 Value-based Payment Study was sent to 5,000 active members of the AAFP. A total of 482 surveys were returned, and 386 were evaluated after a screening process. For a more detailed review, click here.
As of September 30, 2017, Humana has 1.9 million individual Medicare Advantage members (out of 2.8 million total individual MA members) today who are cared for by approximately 51,500 primary care physicians, in more than 900 value-based relationships across 43 states and Puerto Rico. Humana has approximately 66 percent of Humana individual Medicare Advantage members in value-based payment relationships. Humana’s total Medicare Advantage membership is approximately 3.3 million members, which includes members affiliated with providers in value-based and standard Medicare Advantage settings.
About AAFP
Founded in 1947, the AAFP represents 129,000 physicians and medical students nationwide. It is the only medical society devoted solely to primary care.
Family physicians conduct approximately one in five office visits—that’s 192 million visits annually or 48 percent more than the next most visited medical specialty. Today, family physicians provide more care for America’s underserved and rural populations than any other medical specialty. Family medicine’s cornerstone is an ongoing, personal patient-physician relationship focused on integrated care.
To learn more about the specialty of family medicine, the AAFP's positions on issues and clinical care, and for downloadable multi-media highlighting family medicine, visit www.aafp.org/media. For information about health care, health conditions and wellness, please visit the AAFP’s award-winning consumer website, www.familydoctor.org (www.familydoctor.org).
About Humana
Humana Inc. (NYSE: HUM) is committed to helping our millions of medical and specialty members achieve their best health. Our successful history in care delivery and health plan administration is helping us create a new kind of integrated care with the power to improve health and well-being and lower costs. Our efforts are leading to a better quality of life for people with Medicare, families, individuals, military service personnel, and communities at large.
To accomplish that, we support physicians and other health care professionals as they work to deliver the right care in the right place for their patients, our members. Our range of clinical capabilities, resources and tools – such as in-home care, behavioral health, pharmacy services, data analytics and wellness solutions – combine to produce a simplified experience that makes health care easier to navigate and more effective.
More information regarding Humana is available to investors via the Investor Relations page of the company’s web site at www.humana.com, including copies of:
- Annual reports to stockholders
- Securities and Exchange Commission filings
- Most recent investor conference presentations
- Quarterly earnings news releases and conference calls
- Calendar of events
- Corporate Governance information
For Medicare lines of business, Humana is a Medicare Advantage HMO, PPO, and PFFS organization with a Medicare contract. Enrollment in any Humana plan depends on contract renewal. The provider network may change at any time. Impacted members receive notice when necessary.