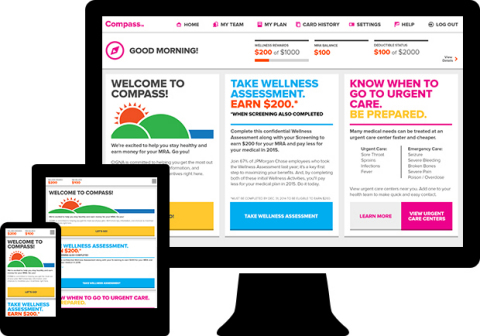
BLOOMFIELD, Conn.--(BUSINESS WIRE)--Global health service company, Cigna (NYSE: CI), announces today the release of Cigna CompassSM, a new web application designed to use anticipatory computing to guide U.S. health plan customers to proactively build their own personal health care team, save money, and get the most from their plans.
Cigna announced the introduction of the new digital experience at the National Business Group on Health’s 2015 Employers' Summit on Health Care Costs and Solutions.
Cigna Compass synthesizes data related to a consumer’s medical plan use, biometric data, incentive information, claims history, and coaching program involvement. Those insights create personalized alerts to notify customers of their top opportunities to improve their health and lower their health care costs.
The tool is designed to simplify the complexity of health care decision making for consumers. In a 2012 study commissioned by Cigna, the research found that consumers ranked “making health care system less confusing through benefit navigation” as their highest priority. Other studies have shown that the likelihood of consumers choosing more efficient health care providers is directly impacted by how cost and quality data are presented**.
Cigna first developed Compass as an innovation initiative for Cigna health plan client JPMorgan Chase. “At JPMorgan Chase, we’re committed to developing a culture of health to help employees and their families make wellness a part of their everyday lives,” says Bernadette Branosky, U.S. Benefits Manager for JPMorgan Chase. “We challenged Cigna to develop a technology-based guidance system to put our people on the path to better health and help them all along their journey. The result is Compass – a digital health care navigation experience that is helping our employees become more aware of their health, improve productivity, and more effectively manage their health care costs.”
“We have to reimagine the health benefits experience for our customers,” says Joan Kennedy, Cigna Vice President for Consumer Engagement. “For the most part consumers have had to find opportunities to maximize their benefits on their own. In contrast, Cigna Compass seeks them out for you by anticipating your needs and preferences giving a targeted choice of solutions.”
By pairing proprietary algorithms with a very clean, simple user experience, Cigna Compass delivers personalized information to customers to:
- Help them build a proactive personal health team of quality, cost-efficient health care professionals and services by guiding customers to stay in network and choose local cost-effective options such as urgent care, preferred labs, and free-standing radiology facilities;
- Educate them on how plan funds work together (HRA/HSA, Incentives, FSA) to lower their out-of-pocket costs;
- Remind them about ongoing reward programs;
- Encourage use of available benefits such as personal health coaches and other programs and resources to improve health;
- Benchmark them against their peer group for the identified opportunity selected and/or how that peer group has benefited from the recommendation (For Example, “Did you know that 70% of people who work with a coach make progress toward their goals?”).
“For example,” Kennedy says, “many Americans do not select a doctor until they really need one, and can make an uninformed and potentially costly choice. To avoid that scenario, Cigna Compass will contact a customer who does not have a designated primary care doctor, and provide a list of nearby in-network health care professionals and facilities based upon the customer’s location before they need to use care.”
Cigna Compass is also designed to reach out to any customer who has an identified opportunity like alerting someone that has not received preventive care with a note that the individual’s plan offers an incentive for a yearly checkup or recommended lab test. As customers make progress toward their health goals and incentive rewards, they can see their updated personal information as well as new recommendations every time they log in, whether from a desktop, tablet, or mobile device.
Early survey results show that 71% of customers find Compass very easy to use, 72% would recommend Compass to a colleague, and 62% said that Compass helps them make better decisions regarding their health.
Cigna Compass is currently being piloted by JPMorgan Chase and will expand to a select number of U.S. employers in 2015. Cigna plans to offer Compass to a broader segment of Cigna's employer sponsored health plan customer base in 2016 and beyond.
MEDIA: For a live demonstration of Cigna Compass, please email joseph.mondy@cigna.com
About Cigna
Cigna Corporation (NYSE: CI) is a global health service company dedicated to helping people improve their health, wellbeing, and sense of security. All products and services are provided exclusively through operating subsidiaries of Cigna Corporation, including Cigna Health and Life Insurance Company, Connecticut General Life Insurance Company, Life Insurance Company of North America, Cigna Life Insurance Company of New York, and their affiliates. Such products and services include an integrated suite of health services, such as medical, dental, behavioral health, pharmacy, and vision care benefits, as well as other related products including group disability, life, and accident coverage. Cigna has sales capability in 30 countries and jurisdictions, with approximately 85 million customer relationships throughout the world. To learn more about Cigna®, including links to follow us on Facebook or Twitter, visit www.cigna.com.
** Health Affairs, “A Well Designed Report on Costs And Quality Can Help Consumers Choose High-Value Health Care” 2012, Appendix page 18