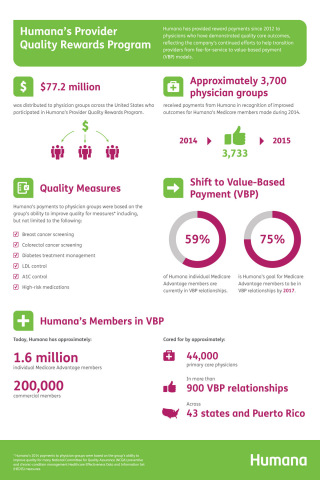
LOUISVILLE, Ky.--(BUSINESS WIRE)--Humana Inc. (NYSE: HUM), today announced that it distributed $77.2 million to physician groups across the United States who participate in Humana’s Provider Quality Rewards Program.
Humana has provided reward payments to physicians who have demonstrated quality care outcomes since 2012, reflecting the company’s continued efforts to help transition providers from fee-for-service to value-based reimbursement models. Currently, approximately 59 percent of Humana individual Medicare Advantage members are attributed to primary care physicians who are participating in value-based relationships. Humana’s goal is to continue growing its programs so that 75 percent of individual Medicare Advantage members are attributed to primary care physicians who are participating in value-based relationships by the end of 2017.
Humana’s Provider Quality Rewards Program is part of Humana’s Accountable Care Continuum, which is a value-based system focused on promoting evidence-based, high-quality care. The Continuum recognizes physician group preparedness for value-based arrangements by offering several levels of participation through programs including Star Rewards, Model Practice, Medical Home and shared savings/full value programs for value-based care.
“The sheer volume of payments distributed through this year’s Provider Quality Rewards Program shows that many physician groups are experiencing success as part of their shift toward value-based care,” said Chip Howard, Humana’s Vice President of Payment Innovation in the Provider Development Center of Excellence. “Humana commends our participating physicians on their success and we are committed to continue supporting their journey to value-based care with the population health management solutions to help them make this transition and ultimately improve the patient care experience.”
Approximately 3,700 physician groups received payments from Humana in recognition of improved outcomes for Humana’s Medicare members made during 2014. Reward settlement finalization takes place in 2015 for the 2014 Rewards Program to allow time for final claims and submission and supplemental data submission.
Humana’s 2014 payments to physician groups were based on their ability to improve quality for many National Committee for Quality Assurance (NCQA) preventive and chronic-condition management Healthcare Effectiveness Data and Information Set (HEDIS) measures including, but not limited to the following:
- Breast cancer screening
- Colorectal cancer screening
- Diabetes treatment management
- LDL control
- A1C control
- High-risk medications
Today, Humana has approximately 1.6 million individual Medicare Advantage and 200,000 commercial members, cared for by approximately 44,000 primary care physicians in more than 900 value-based payment relationships across 43 states and Puerto Rico.
About Humana
Humana Inc., headquartered in Louisville, Ky., is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care. The company’s strategy integrates care delivery, the member experience, and clinical and consumer insights to encourage engagement, behavior change, proactive clinical outreach and wellness for the millions of people we serve across the country.
More information regarding Humana is available to investors via the Investor Relations page of the company’s web site at www.humana.com, including copies of:
- Annual reports to stockholders;
- Securities and Exchange Commission filings;
- Most recent investor conference presentations;
- Quarterly earnings news releases;
- Replays of most recent earnings release conference calls;
- Calendar of events; and
- Corporate Governance information.